MONDAY
On Monday, Zoe was again promoted from the CICU to the CCU/Step-Down Unit. The Lovenox injections started, and Zoe is not a huge fan of being poked with a needle twice a day, but she tolerates it pretty well. I think she is growing accustomed to the torture of her lengthy hospital stay. Her least favorite thing, is when the nurses take her temperature under her armpits, that sends her into a rage. Actually, that might be #2, #1 is hunger. Other than that, she is pretty tolerable. Quite often we hear from the nurses, "she is a really good baby."
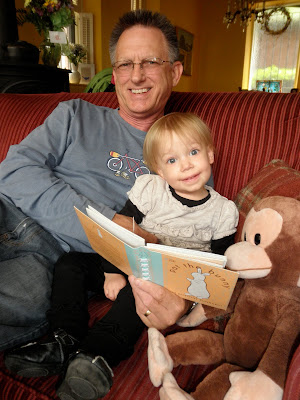
Monday night was Grandpa and Grandma Muenich's, and Emerson's, last night in Philly. They are off to Pittsburgh, PA for Grandma Muenich's Doctoral graduation from Pittsburgh Theological Seminary. Look at the big brain on grandma! In honor of their last night in town, we went for late night cheesesteaks at Jim's Steaks.
We already miss them all, but are so glad they were here to help. Without their sacrifice, picking up and spending three weeks in Philly, this journey would have been exponentially more difficult, if not impossible.
They certainly had some good times with Emmy, and Zoe, while they were here.


We even got one group photo, sort of, Ben Franklin substituted in for Zoe.
TUESDAY
Just another manic Tuesday. What a crazy day!
Tuesday was the day we had to check out of our rental home, however, we obviously need to remain in Philly. Before we left Arizona, we put our name on the Ronald McDonald House waiting list. The Ronald McDonald Houses, located across the country, provide housing to out of town families, whose children are hospitalized, generally for only $15 a night, which includes dinner. The Philadelphia Ronald McDonald house was the original location.
Unfortunately, the house does not take reservations, they have a wait list, but it's based on availability only. You have to call the morning of your desired stay, and hope they have a room.
We had to be out of our rental home by 11:00 a.m., but wouldn't learn our fate at the Ronald McDonald House until 12:00 p.m. So we rented a car, by the hour, loaded two months worth of possessions in it, and drove around around, homeless. Finally, we received a call from the social worker at the Ronald McDonald house. She said she had a room for us. The bad news, however, is that the room is tiny and does not have a full bathroom, only a sink and toilet. The shower is down the hall, in the restrooms - dorm style. Despite the downfalls to the room, we had no choice - we'll take it. So we immediately drove over, checked in, unloaded our bags, then trekked to the hospital in the pouring rain.
Once at the hospital, the doctors kept throwing around the word "discharge." It took us a second to process what that is, not really, but it seemed weird to finally approach an end to this chapter, this hospital stay.
As part of the discharge requirements, we attended a Lovenox class on Tuesday. Essentially, a nurse taught us how to use a needle to draw the medicine out of a vial and how to inject it. We were in a small classroom and we practiced our injections on rubber squares. I'm pretty sure we are Lovenox pros now. Zoe gets the shot twice a day. We were told that we need to give her the shots, until she is discharged. So, when 8:00 p.m. on Tuesday rolled around, we decided I would give the shot first. Stacey stood near Zoe's head and comforted her, while I gave her the shot in the leg. As usual, she was a champ. She has little marks all over her arms and legs from where the twice daily shots have been inserted.
Zoe also had to undergo a car seat test Tuesday. They put her in her car seat for several hours, to simulate long distance traveling. Apparently some kids, when seated in a car seat, for some reason their anatomy causes their respiratory system to be cut off or compromised. If that happens, then the child will need to be transported in a flat car seat. Fortunately, Zoe passed with flying colors.
While at the hospital, the doctors did one final check of Zoe and said she was ready to leave the hospital on Wednesday. Her primary cardiologist at CHOP, however, because we live so far away, wants us to spend a week with Zoe at the Ronald McDonald house. Next week, we will return to the hospital for an echo cardiogram and an office visit. If everything checks out, we will return to Phoenix!!!!
After hanging out with Zoe into the evening, we returned to the Ronald McDonald House to settle in.
Once we were at the house, I received a call from my mom's neighbor who reported that she stopped by her house and was unable to really speak clearly or communicate her thoughts and had stroke like symptoms. So apparently she called 911, and the paramedics came and took my mother to the hospital. She appears to be stable now, but is still in the hospital and I have way too many family members in the hospital right now for my liking.
WEDNESDAY
After a largely sleepless night, Wednesday morning we had to be at the hospital by 7:30 a.m., so Stacey could administer Zoe's Lovenox injection. She was nervous, in fact right as she almost had the needle in the thigh, she paused, but she gave the shot and Zoe even cried less than when I gave it to her. Good job ladies.
So, in between calling the hospital in Arizona, where my mom was admitted, and her doctors, we worked on the logistics for Zoe's discharge. The hospital was supposed to provide boxes and dry ice to ship three tubs of breast milk back to Arizona, however, they were out of boxes, so we had to rent a car and drive to South Philly, to a random dry ice store and buy the special boxes - necessary to ship dry ice. We then went to CVS to pick up Zoe's prescriptions, however, when we arrived they said they did not have any prescriptions for Zoe. So we dropped off the hourly rental car and returned to the hospital. After telling the nurse about CVS, she gave us the prescriptions, five in total, and suggested we run them over to CVS ourselves. After glancing at the prescriptions, Stacey noticed that the Lovenox was missing. The nurse seemed confused and paged case management. Case management, the department that assists with discharge and the related logistics, admitted that they dropped the ball. Because of the holiday weekend, we got lost in the shuffle and the medicine wasn't ordered. They arranged for all the medicines to be available on Thursday. Then will really take Zoe out of the hospital and "home" with us to the Ronny Mac house for the next week or so.
Zoe's discharge from the hospital is bittersweet. Obviously we want to grab her and run out of there with her. But given her condition, it's scary to take her out into the world for the first time, away from the caring and safe hands of the doctors and nurses at CHOP. But its time and we are lucky that Zoe won this battle and is doing as well as she is, despite a couple of set backs.
Tomorrow signifies the beginning of a new chapter in Zoe's journey.














